January 24, 2008
Camera in a pill offers cheaper, easier window on your insides
What if swallowing a pill with a camera could detect the earliest signs of cancer? The tiny camera is designed to take high-quality, color pictures in confined spaces. Such a device could find warning signs of esophageal cancer, the fastest growing cancer in the United States.
A fundamentally new design has created a smaller endoscope that is more comfortable for the patient and cheaper to use than current technology. Its first use on a human, scanning for early signs of esophageal cancer, will be reported in an upcoming issue of IEEE Transactions on Biomedical Engineering.
“Our technology is completely different from what’s available now. This could be the foundation for the future of endoscopy,” said lead author Eric Seibel, a University of Washington research associate professor of mechanical engineering.
In the past 30 years diagnoses of esophageal cancer have more than tripled. The esophagus is the section of digestive tract that moves food from the throat down to the stomach. Esophageal cancer often follows a condition called Barrett’s esophagus, a noticeable change in the esophageal lining. Patients with Barrett’s esophagus can be healed, avoiding the deadly esophageal cancer. But because internal scans are expensive most people don’t find out they have the condition until it’s progressed to cancer, and by that stage the survival rate is less than 15 percent.
“These are needless deaths,” Seibel said. “Any screen that detected whether you had a treatable condition before it had turned into cancer would save lives.”
An endoscope is a flexible camera that travels into the body’s cavities to directly investigate the digestive tract, colon or throat. Most of today’s endoscopes capture the image using a traditional approach where each part of the camera captures a different section of the image. These tools are long, flexible cords about 9 mm wide, about the width of a human fingernail. Because the cord is so wide patients must be sedated during the scan.
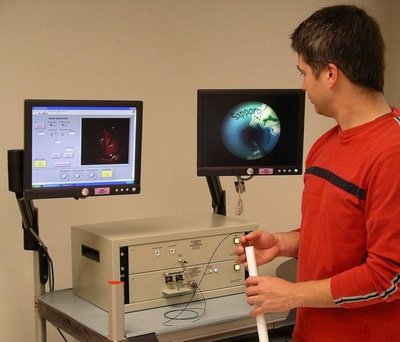
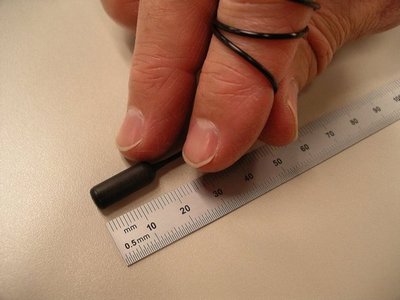
The scanning endoscope developed at the UW is fundamentally different. It consists of just a single optical fiber for illumination and six fibers for collecting light, all encased in a pill. Seibel acted as the human volunteer in the first test of the UW device. He reports that it felt like swallowing a regular pill, and the tether, which is 1.4 mm wide, did not bother him.
Once swallowed, an electric current flowing through the UW endoscope causes the fiber to bounce back and forth so that its lone electronic eye sees the whole scene, one pixel at a time. At the same time the fiber spins and its tip projects red, green and blue laser light. The image processing then combines all this information to create a two-dimensional color picture.
In the tested model the fiber swings 5,000 times per second, creating 15 color pictures per second. The resolution is better than 100 microns, or more than 500 lines per inch. Although conventional endoscopes produce images at higher resolution, the tethered-capsule endoscope is designed specifically for low-cost screening.
Using the scanning device is cheap because it’s so small it doesn’t require anesthesia and sedation, which increase the cost of the traditional procedure.
“The procedure is so easy I could imagine it being done in a shopping mall,” Seibel said.
A wireless scope manufactured by a different group, originally designed to pass through the body and detect intestinal cancer, is now being marketed for esophageal cancer screening. The competing technology comes in a pill about the width of an adult fingernail and twice as long. By contrast, the UW’s scanning fiber endoscope’s dimensions are about half as big and the device fits inside a standard pill capsule. The pill could be even smaller, Seibel said, but the researchers chose a size that would be easy to handle and swallow.
Another disadvantage of wireless capsules is they only allow a single fly-by view.
“You have no control over the other pill once it’s swallowed. It just flutters down,” Seibel said. But since the UW scope is tethered, the doctor can move it up and down along the region of interest.
Only a small percentage of people who get Barrett’s esophagus, about 5 percent to 10 percent, develop cancer. So any screening method must have a low price to be cost-effective.
“The next big challenge is to make this cheaply,” Seibel said. The researchers are negotiating a contract to commercialize the technology. In the future they hope to not only take pictures, but also deliver treatments through the device, and to apply it to other diseases.
The research was funded by the National Cancer Institute and Pentax Corp. Early funding was provided by the Whitaker Foundation and the Washington Technology Center. Co-authors at the UW are Drs. Michael Kimmey and Jason Dominitz in gastroenterology at the UW Medical Center; Richard Johnston, C. David Melville and Cameron Lee in mechanical engineering; Steve Seitz in computer science and engineering; and Robert Carroll, now in electrical engineering and computer science at the University of California, Berkeley.
###
For more information, contact Seibel at (206) 616-1486 or eseibel@u.washington.edu.